Antibiotics are a crucial tool in treating bacterial infections in dental clinics. However, excessive and inappropriate use of antibiotics can lead to antibiotic resistance, which has become a significant public health concern.
Antibiotic resistance is a growing problem worldwide and can reduce the effectiveness of antibiotics, making it more difficult to treat bacterial infections. It is essential to understand when to use antibiotics by following the evidence-based dental antibiotic guidelines set forth by the American Dental Association (ADA).
Antibiotic Resistance in Dentistry
Antibiotic Resistance: How Does it Occur?
Resistance occurs when bacteria develop the ability to withstand the effects of antibiotics, making them less effective in treating infections. Overusing or misusing broad-spectrum medications like Clavulin (Amoxicillin/Clavulanate) can lead to the evolution of antibiotic-resistant bacteria. This can cause infections that are more severe, longer hospital stays, increased healthcare costs, and even death.
What Are The Consequences of Antibiotic Resistance?
As a clinical pharmacist in the hospital setting, I have seen firsthand the unfortunate consequences of repeated antibiotic use. The insidious part about resistance is that it is not isolated to one type of infection or person.
One example I have seen is a patient who had been treated repeatedly for cellulitis and developed pneumonia that was cultured for methicillin-resistant staph aureus (MRSA). Unfortunately, this patient was not isolated soon enough and transmitted MRSA pneumonia to other patients throughout the ward.
The Importance of Proper Antibiotic Use in Dental Practice
Antibiotic resistance might seem like an isolated occurrence in hospitals, but treating patients with broad-spectrum medications like Clavulin can lead to serious consequences in the community as well. As a community healthcare provider, it is important for dentists to understand proper antibiotic use and follow the guidelines set forth by the ADA to help prevent bacterial resistance and protect your patient's health.
Antibiotic Misuse in Dentistry
Let’s address the elephant in the room: there is growing concern about the overuse of antibiotics in dental clinics. Some dentists prescribe antibiotics as a precautionary measure, even when there is no clear indication of infection. This can lead to unnecessary exposure and an increased risk of resistance.
Careful evaluation of each patient's condition is crucial in determining whether infection control is necessary. Alternative treatments, such as pain management and localized treatment, should be considered before prescribing antibiotics.
In the following section, we will explore when and how antibiotics should be used in the dental setting, as described by the ADA.
American Dental Association: Dental Antibiotic Guidelines
The ADA has established comprehensive antibiotic guidelines for the prevention and treatment of dental infections. These guidelines provide a framework for prescribing antibiotics in a manner that prevents the development of bacterial resistance.
According to the ADA guidelines, antibiotics should only be prescribed for specific conditions, such as acute oral infections, prophylaxis in patients with certain heart conditions, and in cases where there is a risk of infection spreading to other parts of the body. Antibiotics should not be prescribed for routine dental procedures, such as fillings or extractions unless the patient has a pre-existing condition that puts them at risk of infection.
Unfortunately, the ADA guidelines are a bit dense and don't have a good summary. So instead of just sending you to read through the full articles, we have compiled the recommendations set out by the ADA for your convenience:
Dental Antibiotic Prophylaxis
Evidence Based Recommendations for the PREVENTION of ENDOCARDITIS
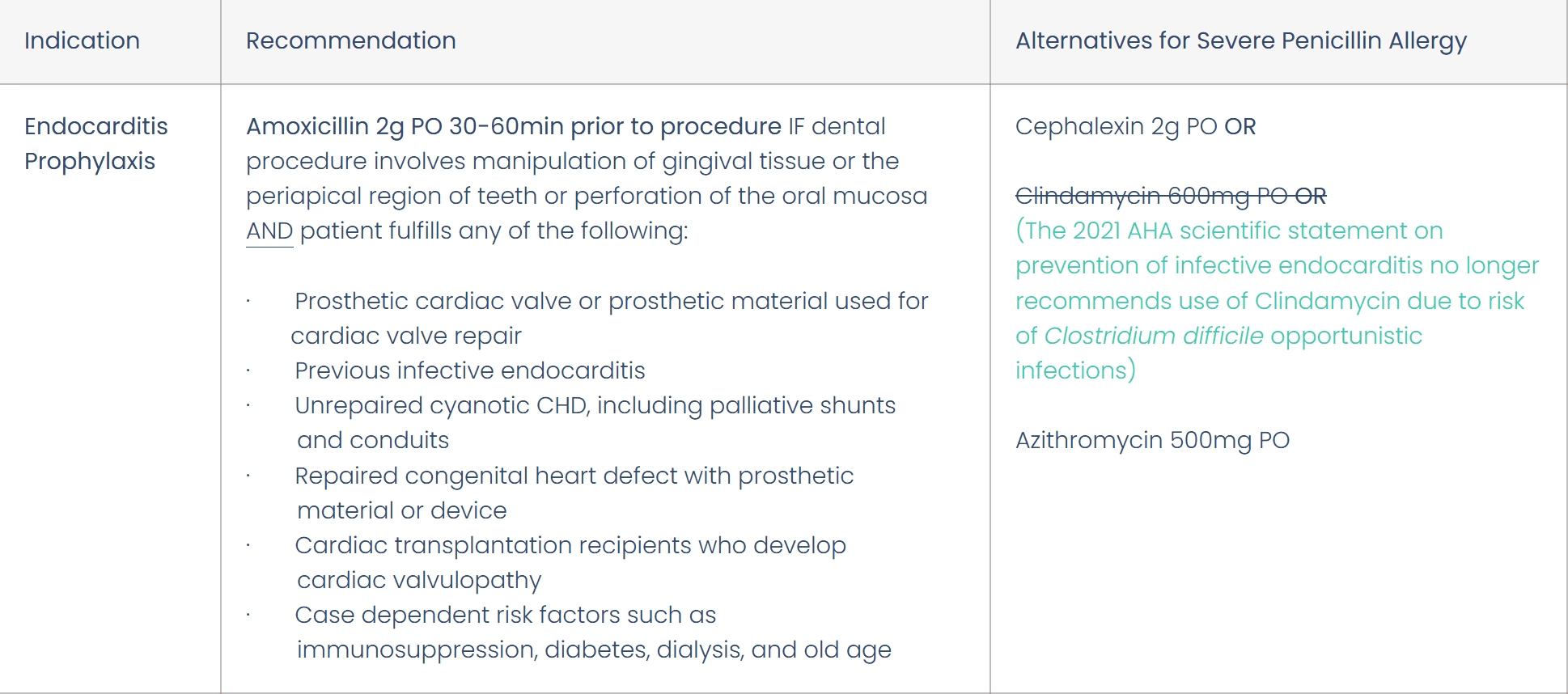
Prevention of infective endocarditis: Guidelines from the American Heart Association
Note: There is currently NO evidence supporting antibiotic prophylaxis for PREVENTION of PROSTHETIC JOINT INFECTIONS
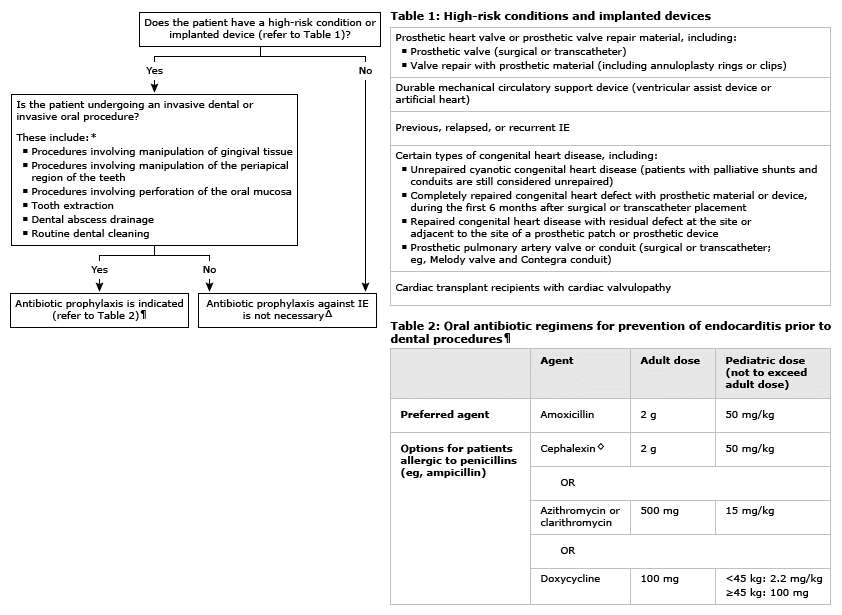
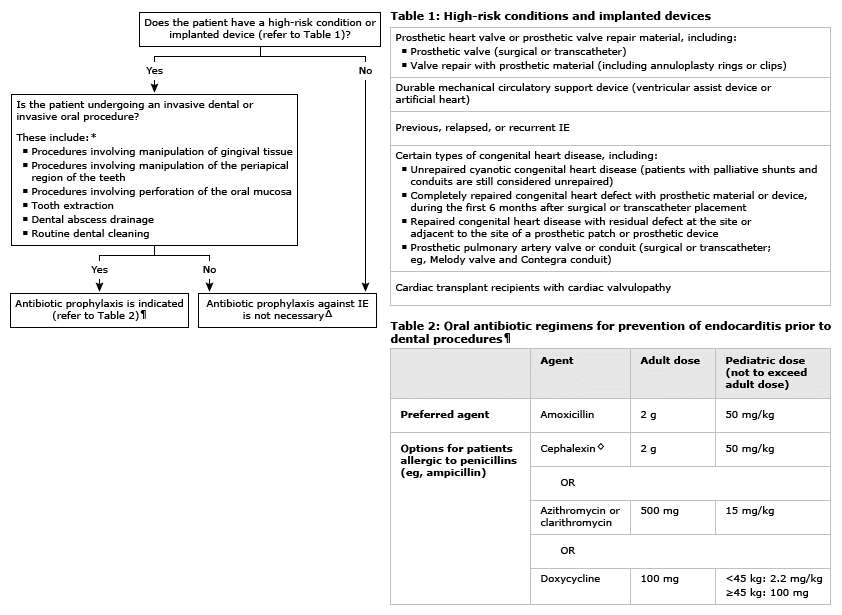
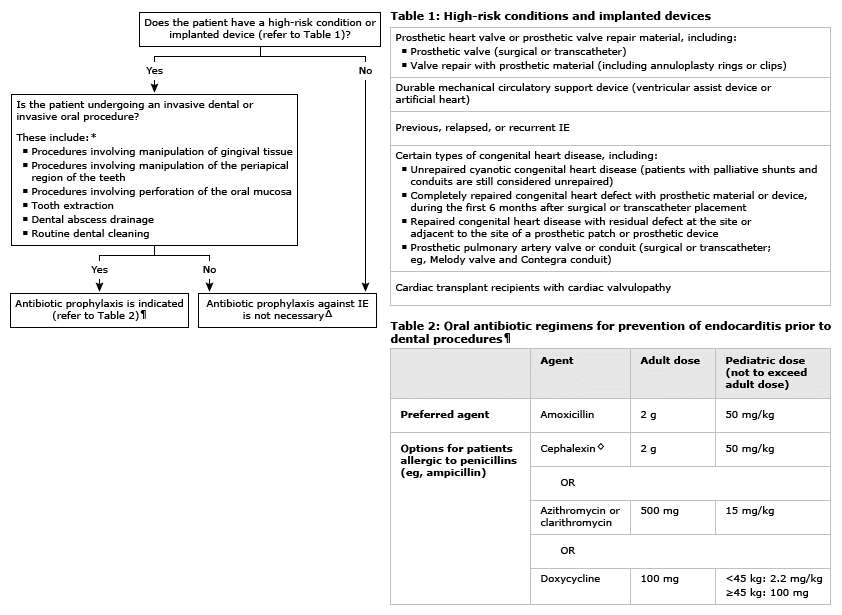
This is also a nice decision-making tree from UpToDate to help with visualization:
Dental Antibiotic Treatment
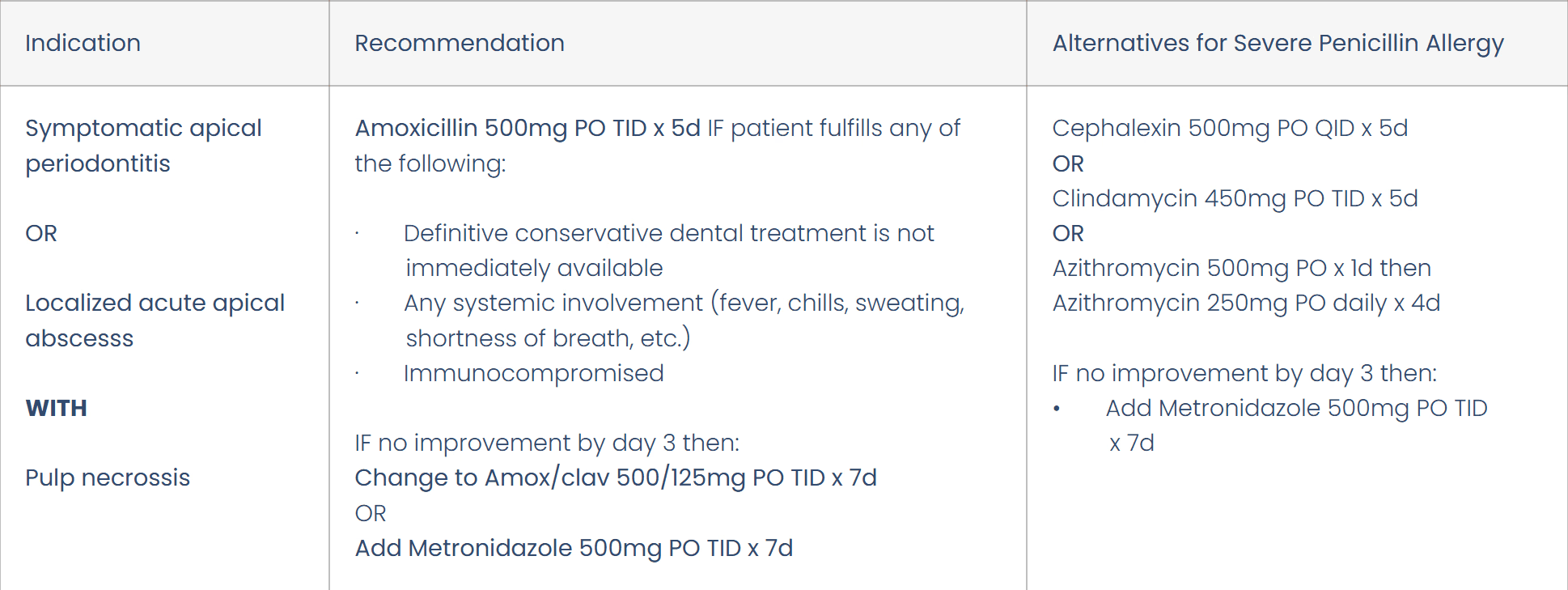
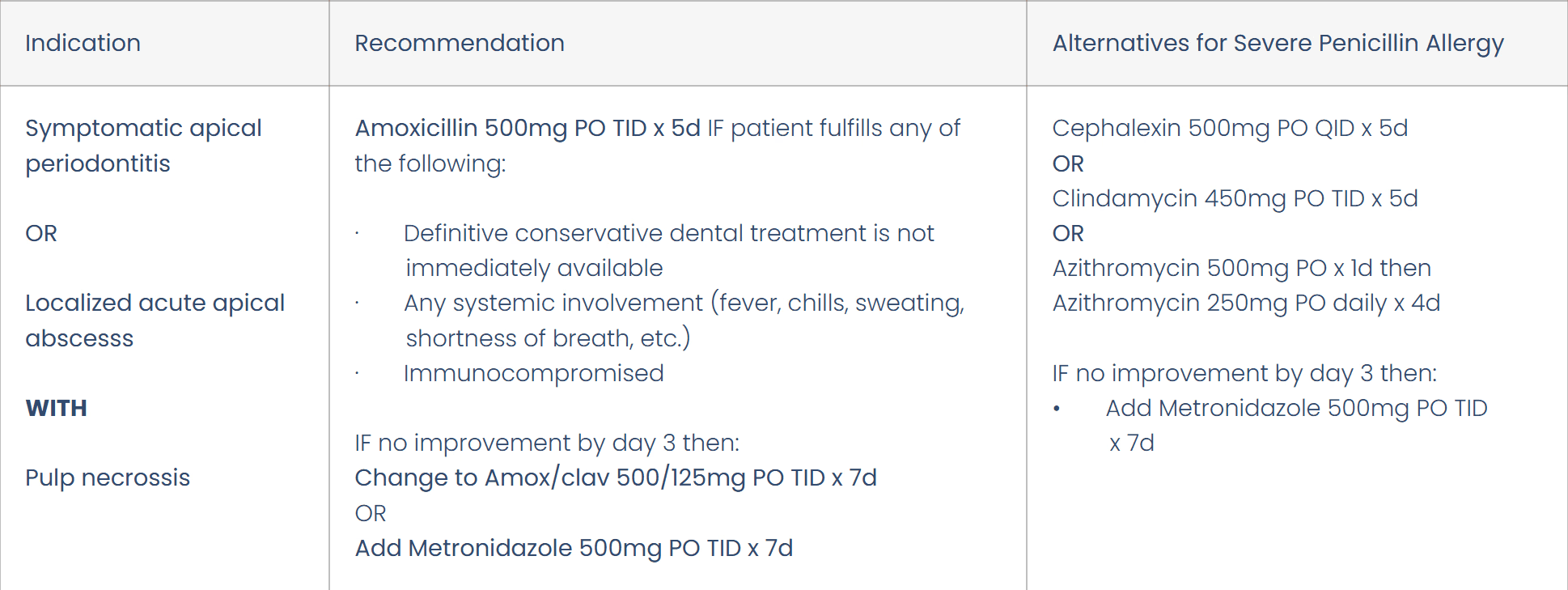
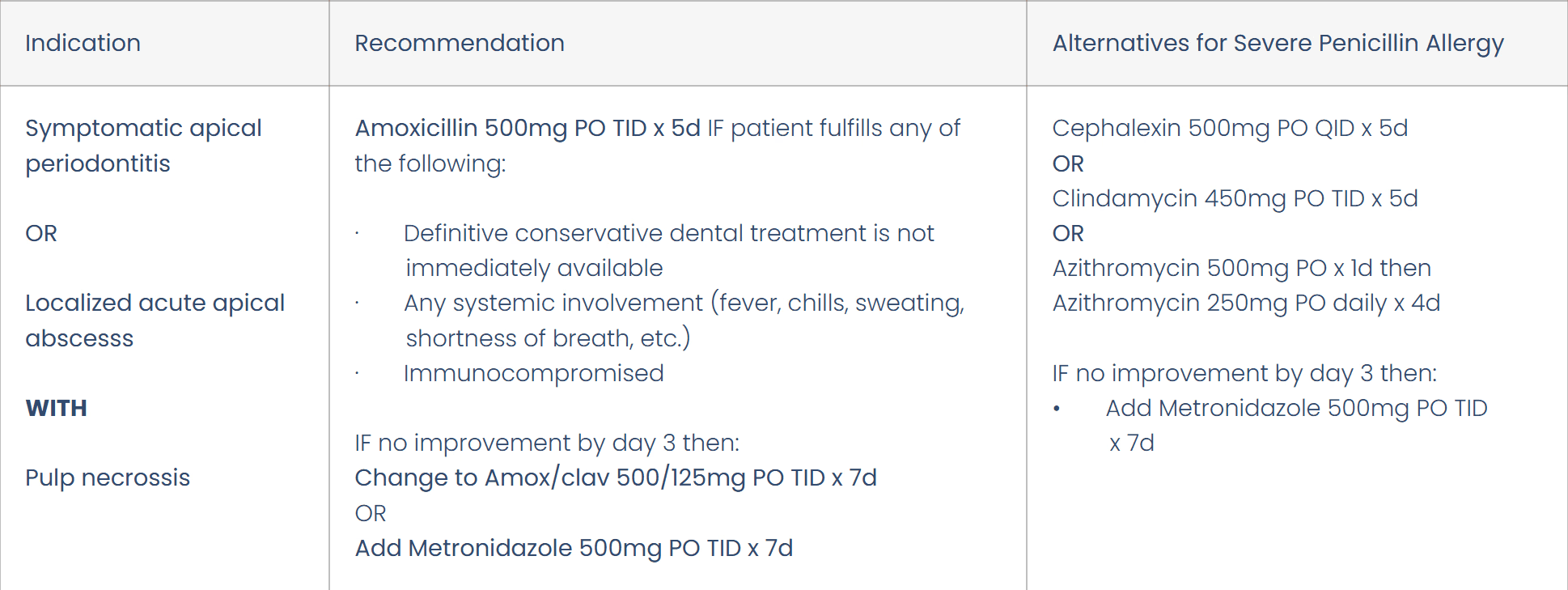
Evidence-Based Recommendations for ACTIVE INFECTIONS
Feel free to use these resources at your dental clinic, and consider downloading the DentalRx app to access these guidelines at any time in your practice!
The Role of Dentists in Antimicrobial Stewardship
Dentists have a critical role to play in antimicrobial stewardship, which is the responsible use of these agents to preserve their effectiveness. Dentists can contribute to antibiotic stewardship by following the ADA guidelines, carefully evaluating each patient's condition, and prescribing antibiotics only when necessary.
To help in this endeavour, we have created the mobile and web application DentalRx. Dentists can use DentalRx to research antibiotics, so that they may safely prescribe, and ultimately provide better patient care. All this without having to search the internet for updated guidelines or deciphering outdated resources.
Dentists can also educate their patients about the proper use of medications and the importance of completing the full course of treatment. By doing so, you can help prevent the development of bacterial resistance and preserve the effectiveness of antibiotics.
Conclusion
Antibiotics play an essential role in the treatment of oral infections, but their use should be carefully evaluated to prevent bacterial resistance. The guidelines set out by the ADA are a useful tool for you to use, but should not overturn your clinical judgment. By practicing responsible prescribing, we can help to preserve the effectiveness of antibiotics for future generations.
Continuing to stay updated with the latest research and guidelines like the ones outlined here ensures that you are providing the best possible care to your patients while also providing best practices for harm prevention.
References
Chu, V. H., Otto, C. M., Edwards, M. S., Baron, E. L., & Yeon, S. B. (2024). Prevention of endocarditis: Antibiotic prophylaxis and other measures. UpToDate. Retrieved from https://www.uptodate.com/contents/prevention-of-endocarditis-antibiotic-prophylaxis-and-other-measures
Lockhart, P. B., Tampi, M. P., Abt, E., Aminoshariae, A., Durkin, M. J., Fouad, A. F., Gopal, P., Hatten, B. W., Kennedy, E., Lang, M. S., Patton, L. L., Paumier, T., Suda, K. J., Pilcher, L., Urquhart, O., O’Brien, K. K., & Carrasco-Labra, A. (2019). Evidence-based clinical practice guideline on antibiotic use for the urgent management of pulpal- and periapical-related dental pain and intraoral swelling: A report from the American Dental Association. Journal of the American Dental Association, 150(11), 906-921.e12. Retrieved from https://jada.ada.org/article/S0002-8177(19)30617-8/fulltext
Wilson, W., Taubert, K. A., Gewitz, M., Lockhart, P. B., Baddour, L. M., Levison, M., Bolger, A., Cabell, C. H., Takahashi, M., Baltimore, R. S., Newburger, J. W., Strom, B. L., Tani, L. Y., Gerber, M., Bonow, R. O., Pallasch, T., Shulman, S. T., Rowley, A. H., Burns, J. C., … Durack, D. T. (2007). Prevention of infective endocarditis: Guidelines from the American Heart Association. Journal of the American Dental Association, 138(6), 739-745. Retrieved from https://jada.ada.org/article/S0002-8177(14)62745-8/fulltext
Antibiotics are a crucial tool in treating bacterial infections in dental clinics. However, excessive and inappropriate use of antibiotics can lead to antibiotic resistance, which has become a significant public health concern.
Antibiotic resistance is a growing problem worldwide and can reduce the effectiveness of antibiotics, making it more difficult to treat bacterial infections. It is essential to understand when to use antibiotics by following the evidence-based dental antibiotic guidelines set forth by the American Dental Association (ADA).
Antibiotic Resistance in Dentistry
Antibiotic Resistance: How Does it Occur?
Resistance occurs when bacteria develop the ability to withstand the effects of antibiotics, making them less effective in treating infections. Overusing or misusing broad-spectrum medications like Clavulin (Amoxicillin/Clavulanate) can lead to the evolution of antibiotic-resistant bacteria. This can cause infections that are more severe, longer hospital stays, increased healthcare costs, and even death.
What Are The Consequences of Antibiotic Resistance?
As a clinical pharmacist in the hospital setting, I have seen firsthand the unfortunate consequences of repeated antibiotic use. The insidious part about resistance is that it is not isolated to one type of infection or person.
One example I have seen is a patient who had been treated repeatedly for cellulitis and developed pneumonia that was cultured for methicillin-resistant staph aureus (MRSA). Unfortunately, this patient was not isolated soon enough and transmitted MRSA pneumonia to other patients throughout the ward.
The Importance of Proper Antibiotic Use in Dental Practice
Antibiotic resistance might seem like an isolated occurrence in hospitals, but treating patients with broad-spectrum medications like Clavulin can lead to serious consequences in the community as well. As a community healthcare provider, it is important for dentists to understand proper antibiotic use and follow the guidelines set forth by the ADA to help prevent bacterial resistance and protect your patient's health.
Antibiotic Misuse in Dentistry
Let’s address the elephant in the room: there is growing concern about the overuse of antibiotics in dental clinics. Some dentists prescribe antibiotics as a precautionary measure, even when there is no clear indication of infection. This can lead to unnecessary exposure and an increased risk of resistance.
Careful evaluation of each patient's condition is crucial in determining whether infection control is necessary. Alternative treatments, such as pain management and localized treatment, should be considered before prescribing antibiotics.
In the following section, we will explore when and how antibiotics should be used in the dental setting, as described by the ADA.
American Dental Association: Dental Antibiotic Guidelines
The ADA has established comprehensive antibiotic guidelines for the prevention and treatment of dental infections. These guidelines provide a framework for prescribing antibiotics in a manner that prevents the development of bacterial resistance.
According to the ADA guidelines, antibiotics should only be prescribed for specific conditions, such as acute oral infections, prophylaxis in patients with certain heart conditions, and in cases where there is a risk of infection spreading to other parts of the body. Antibiotics should not be prescribed for routine dental procedures, such as fillings or extractions unless the patient has a pre-existing condition that puts them at risk of infection.
Unfortunately, the ADA guidelines are a bit dense and don't have a good summary. So instead of just sending you to read through the full articles, we have compiled the recommendations set out by the ADA for your convenience:
Dental Antibiotic Prophylaxis
Evidence Based Recommendations for the PREVENTION of ENDOCARDITIS
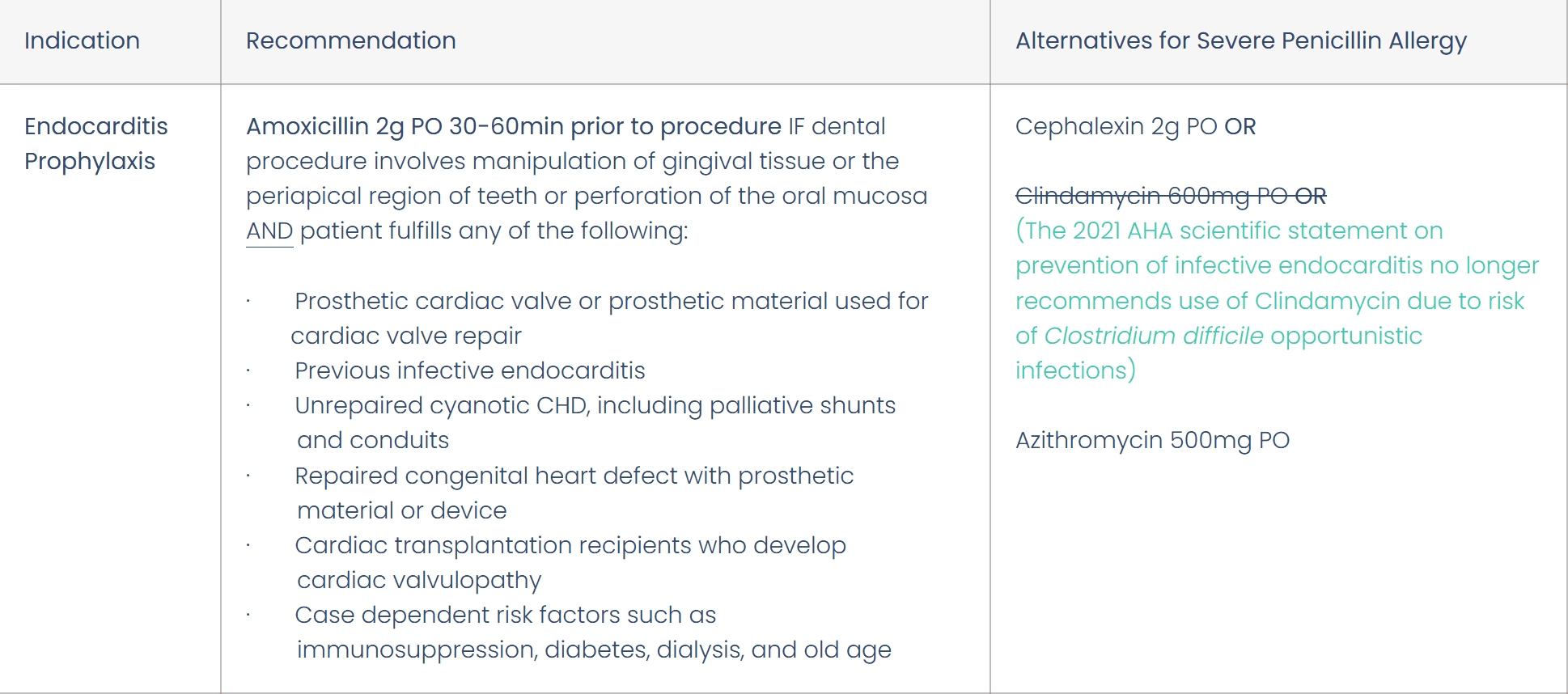
Prevention of infective endocarditis: Guidelines from the American Heart Association
Note: There is currently NO evidence supporting antibiotic prophylaxis for PREVENTION of PROSTHETIC JOINT INFECTIONS
This is also a nice decision-making tree from UpToDate to help with visualization:
Dental Antibiotic Treatment
Evidence-Based Recommendations for ACTIVE INFECTIONS
Feel free to use these resources at your dental clinic, and consider downloading the DentalRx app to access these guidelines at any time in your practice!
The Role of Dentists in Antimicrobial Stewardship
Dentists have a critical role to play in antimicrobial stewardship, which is the responsible use of these agents to preserve their effectiveness. Dentists can contribute to antibiotic stewardship by following the ADA guidelines, carefully evaluating each patient's condition, and prescribing antibiotics only when necessary.
To help in this endeavour, we have created the mobile and web application DentalRx. Dentists can use DentalRx to research antibiotics, so that they may safely prescribe, and ultimately provide better patient care. All this without having to search the internet for updated guidelines or deciphering outdated resources.
Dentists can also educate their patients about the proper use of medications and the importance of completing the full course of treatment. By doing so, you can help prevent the development of bacterial resistance and preserve the effectiveness of antibiotics.
Conclusion
Antibiotics play an essential role in the treatment of oral infections, but their use should be carefully evaluated to prevent bacterial resistance. The guidelines set out by the ADA are a useful tool for you to use, but should not overturn your clinical judgment. By practicing responsible prescribing, we can help to preserve the effectiveness of antibiotics for future generations.
Continuing to stay updated with the latest research and guidelines like the ones outlined here ensures that you are providing the best possible care to your patients while also providing best practices for harm prevention.
References
Chu, V. H., Otto, C. M., Edwards, M. S., Baron, E. L., & Yeon, S. B. (2024). Prevention of endocarditis: Antibiotic prophylaxis and other measures. UpToDate. Retrieved from https://www.uptodate.com/contents/prevention-of-endocarditis-antibiotic-prophylaxis-and-other-measures
Lockhart, P. B., Tampi, M. P., Abt, E., Aminoshariae, A., Durkin, M. J., Fouad, A. F., Gopal, P., Hatten, B. W., Kennedy, E., Lang, M. S., Patton, L. L., Paumier, T., Suda, K. J., Pilcher, L., Urquhart, O., O’Brien, K. K., & Carrasco-Labra, A. (2019). Evidence-based clinical practice guideline on antibiotic use for the urgent management of pulpal- and periapical-related dental pain and intraoral swelling: A report from the American Dental Association. Journal of the American Dental Association, 150(11), 906-921.e12. Retrieved from https://jada.ada.org/article/S0002-8177(19)30617-8/fulltext
Wilson, W., Taubert, K. A., Gewitz, M., Lockhart, P. B., Baddour, L. M., Levison, M., Bolger, A., Cabell, C. H., Takahashi, M., Baltimore, R. S., Newburger, J. W., Strom, B. L., Tani, L. Y., Gerber, M., Bonow, R. O., Pallasch, T., Shulman, S. T., Rowley, A. H., Burns, J. C., … Durack, D. T. (2007). Prevention of infective endocarditis: Guidelines from the American Heart Association. Journal of the American Dental Association, 138(6), 739-745. Retrieved from https://jada.ada.org/article/S0002-8177(14)62745-8/fulltext
Antibiotics are a crucial tool in treating bacterial infections in dental clinics. However, excessive and inappropriate use of antibiotics can lead to antibiotic resistance, which has become a significant public health concern.
Antibiotic resistance is a growing problem worldwide and can reduce the effectiveness of antibiotics, making it more difficult to treat bacterial infections. It is essential to understand when to use antibiotics by following the evidence-based dental antibiotic guidelines set forth by the American Dental Association (ADA).
Antibiotic Resistance in Dentistry
Antibiotic Resistance: How Does it Occur?
Resistance occurs when bacteria develop the ability to withstand the effects of antibiotics, making them less effective in treating infections. Overusing or misusing broad-spectrum medications like Clavulin (Amoxicillin/Clavulanate) can lead to the evolution of antibiotic-resistant bacteria. This can cause infections that are more severe, longer hospital stays, increased healthcare costs, and even death.
What Are The Consequences of Antibiotic Resistance?
As a clinical pharmacist in the hospital setting, I have seen firsthand the unfortunate consequences of repeated antibiotic use. The insidious part about resistance is that it is not isolated to one type of infection or person.
One example I have seen is a patient who had been treated repeatedly for cellulitis and developed pneumonia that was cultured for methicillin-resistant staph aureus (MRSA). Unfortunately, this patient was not isolated soon enough and transmitted MRSA pneumonia to other patients throughout the ward.
The Importance of Proper Antibiotic Use in Dental Practice
Antibiotic resistance might seem like an isolated occurrence in hospitals, but treating patients with broad-spectrum medications like Clavulin can lead to serious consequences in the community as well. As a community healthcare provider, it is important for dentists to understand proper antibiotic use and follow the guidelines set forth by the ADA to help prevent bacterial resistance and protect your patient's health.
Antibiotic Misuse in Dentistry
Let’s address the elephant in the room: there is growing concern about the overuse of antibiotics in dental clinics. Some dentists prescribe antibiotics as a precautionary measure, even when there is no clear indication of infection. This can lead to unnecessary exposure and an increased risk of resistance.
Careful evaluation of each patient's condition is crucial in determining whether infection control is necessary. Alternative treatments, such as pain management and localized treatment, should be considered before prescribing antibiotics.
In the following section, we will explore when and how antibiotics should be used in the dental setting, as described by the ADA.
American Dental Association: Dental Antibiotic Guidelines
The ADA has established comprehensive antibiotic guidelines for the prevention and treatment of dental infections. These guidelines provide a framework for prescribing antibiotics in a manner that prevents the development of bacterial resistance.
According to the ADA guidelines, antibiotics should only be prescribed for specific conditions, such as acute oral infections, prophylaxis in patients with certain heart conditions, and in cases where there is a risk of infection spreading to other parts of the body. Antibiotics should not be prescribed for routine dental procedures, such as fillings or extractions unless the patient has a pre-existing condition that puts them at risk of infection.
Unfortunately, the ADA guidelines are a bit dense and don't have a good summary. So instead of just sending you to read through the full articles, we have compiled the recommendations set out by the ADA for your convenience:
Dental Antibiotic Prophylaxis
Evidence Based Recommendations for the PREVENTION of ENDOCARDITIS
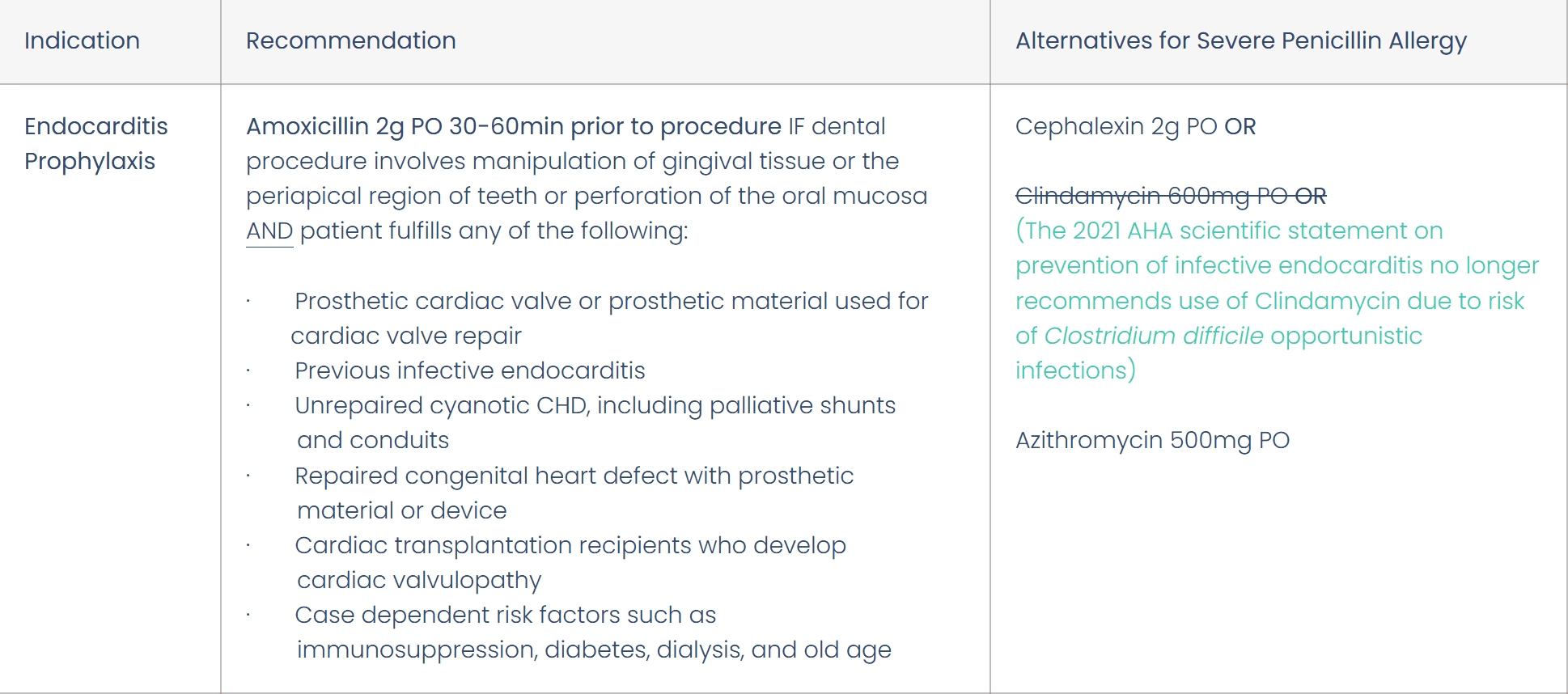
Prevention of infective endocarditis: Guidelines from the American Heart Association
Note: There is currently NO evidence supporting antibiotic prophylaxis for PREVENTION of PROSTHETIC JOINT INFECTIONS
This is also a nice decision-making tree from UpToDate to help with visualization:
Dental Antibiotic Treatment
Evidence-Based Recommendations for ACTIVE INFECTIONS
Feel free to use these resources at your dental clinic, and consider downloading the DentalRx app to access these guidelines at any time in your practice!
The Role of Dentists in Antimicrobial Stewardship
Dentists have a critical role to play in antimicrobial stewardship, which is the responsible use of these agents to preserve their effectiveness. Dentists can contribute to antibiotic stewardship by following the ADA guidelines, carefully evaluating each patient's condition, and prescribing antibiotics only when necessary.
To help in this endeavour, we have created the mobile and web application DentalRx. Dentists can use DentalRx to research antibiotics, so that they may safely prescribe, and ultimately provide better patient care. All this without having to search the internet for updated guidelines or deciphering outdated resources.
Dentists can also educate their patients about the proper use of medications and the importance of completing the full course of treatment. By doing so, you can help prevent the development of bacterial resistance and preserve the effectiveness of antibiotics.
Conclusion
Antibiotics play an essential role in the treatment of oral infections, but their use should be carefully evaluated to prevent bacterial resistance. The guidelines set out by the ADA are a useful tool for you to use, but should not overturn your clinical judgment. By practicing responsible prescribing, we can help to preserve the effectiveness of antibiotics for future generations.
Continuing to stay updated with the latest research and guidelines like the ones outlined here ensures that you are providing the best possible care to your patients while also providing best practices for harm prevention.
References
Chu, V. H., Otto, C. M., Edwards, M. S., Baron, E. L., & Yeon, S. B. (2024). Prevention of endocarditis: Antibiotic prophylaxis and other measures. UpToDate. Retrieved from https://www.uptodate.com/contents/prevention-of-endocarditis-antibiotic-prophylaxis-and-other-measures
Lockhart, P. B., Tampi, M. P., Abt, E., Aminoshariae, A., Durkin, M. J., Fouad, A. F., Gopal, P., Hatten, B. W., Kennedy, E., Lang, M. S., Patton, L. L., Paumier, T., Suda, K. J., Pilcher, L., Urquhart, O., O’Brien, K. K., & Carrasco-Labra, A. (2019). Evidence-based clinical practice guideline on antibiotic use for the urgent management of pulpal- and periapical-related dental pain and intraoral swelling: A report from the American Dental Association. Journal of the American Dental Association, 150(11), 906-921.e12. Retrieved from https://jada.ada.org/article/S0002-8177(19)30617-8/fulltext
Wilson, W., Taubert, K. A., Gewitz, M., Lockhart, P. B., Baddour, L. M., Levison, M., Bolger, A., Cabell, C. H., Takahashi, M., Baltimore, R. S., Newburger, J. W., Strom, B. L., Tani, L. Y., Gerber, M., Bonow, R. O., Pallasch, T., Shulman, S. T., Rowley, A. H., Burns, J. C., … Durack, D. T. (2007). Prevention of infective endocarditis: Guidelines from the American Heart Association. Journal of the American Dental Association, 138(6), 739-745. Retrieved from https://jada.ada.org/article/S0002-8177(14)62745-8/fulltext