Ensuring Dental Safety for Pregnant Patients
Managing dental care for pregnant patients is a complex yet crucial responsibility. Dental professionals must navigate treatment options with caution, especially when prescribing medications. The goal of this article is to provide an evidence-based guide to facilitate safer and more effective treatment plans for pregnant patients.
Revised Drug Pregnancy Categories in Dental Practice
Previously, the FDA provided drug pregnancy categories for healthcare professionals to make decisions about drug therapy. These categories provided a framework for evaluating the risks and benefits of medication use during pregnancy.
In 2015, the Food and Drug Administration (FDA) eliminated the standard pregnancy category letters (A, B, C, D, and X) for prescription medications. The new recommendations now take the form of drug labeling that provides greater detail but also introduces increased complexity.
The FDA’s transition from pregnancy category letters to more comprehensive labeling requires dentists to assess medication risks carefully. This change reflects a need for a deeper understanding of medication safety in pregnancy.
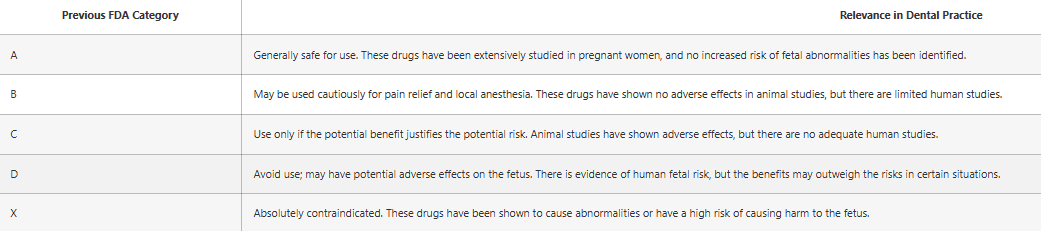
Following the FDA's changes, health professionals should no longer base their decisions on pregnancy categories. Instead, they should adopt a nuanced approach to each medication, carefully assessing all available evidence.
Continuing in this article, we will be summarizing the evidence that we have collected for your convenience.
Medications Commonly Used in Dental Practice
The following table from the 2012 Oral Health Care During Pregnancy Expert Workgroup is particularly helpful as a quick reference when prescribing medications for pregnant dental patients. It provides a concise overview of the commonly prescribed medications in dentistry.
Analgesics
Acetaminophen
May be used during pregnancy.
Oral pain can often be managed with non-opioid medication.
Acetaminophen with Codeine
During pregnancy, this medication should be used only when clearly needed.
It may slightly increase the risk of birth defects if used during the first two months of pregnancy.
Prescribed in high doses near the expected delivery date may harm the unborn baby.
To lessen the risk, prescribe the smallest effective dose for the shortest possible time.
Babies born to mothers who use this drug for a long time may develop severe (possibly fatal) withdrawal symptoms.
Aspirin
First trimester: Avoid use.
Second trimester (13–20 weeks): May use for a short duration (48–72 hours).
Second trimester (20–27 weeks): Limit use.
Third trimester: Avoid use.
Ibuprofen and Naproxen
Second trimester, after 20 weeks: Avoid use.
Third trimester: Avoid use.
Antibiotics
Amoxicillin, Cephalosporins, Clindamycin, Metronidazole, Penicillin
May be used during pregnancy.
Ciprofloxacin, Levofloxacin, Moxifloxacin
Avoid during pregnancy.
Tetracycline
Never use during pregnancy.
Anesthetics
Local Anesthetics with Epinephrine (e.g., Bupivacaine, Lidocaine, Mepivacaine)
May be used during pregnancy.
General Anesthesia
Consult a prenatal care health professional before use.
Limit duration of exposure to less than 3 hours, especially in the third trimester.
Antimicrobials
Cetylpyridinium Chloride Mouth Rinse, Chlorhexidine Mouth Rinse, Xylitol
May be used during pregnancy.
Use alcohol-free products during pregnancy.
Updates Since the Working Group
The list above was published in 2012 by the expert working group, and since then additional commentary has been provided on certain medications used in pregnancy.
Nitrous Oxide: It is recommended that pregnant individuals avoid exposure to nitrous oxide. The National Institute of Occupational Safety and Health (NIOSH), recommends exposure limits of N2O concentrations in dental operations to approximately 25 ppm during analgesia administration.
Meperidine: Meperidine should not be used in pregnant women before the onset of labor unless the physician determines that the potential benefits outweigh the associated risks. Safe use in pregnancy before labor has not been established relative to possible adverse effects on fetal development. Available data with DEMEROL Injection are insufficient to inform a drug-associated risk for major birth defects and miscarriage.
Morphine: Based on the studies reviewed, it is not known if morphine increases the chance of pregnancy-related problems such as preterm delivery (birth before week 37) or low birth weight (weighing less than 5 pounds, 8 ounces [2500 grams] at birth).
One case of high heart rate (tachycardia) in a near-term (36-week) fetus was described after a person who was pregnant was given morphine for kidney pain (renal colic). A person using morphine for chronic pain control in their third trimester of pregnancy was observed to have constriction in the blood vessels of the placenta, also known as placental vasoconstriction.
Bupivacaine, Mepivacaine: These local anesthetics should not be used in pregnant women before the onset of labor unless the physician determines that the potential benefits outweigh the possible risks. Fetal bradycardia with Mepivacaine & Bupivacaine is a potential risk.
Special Considerations in Dental Practice
Timing of Treatments
First Trimester: Avoid non-emergency treatments due to the sensitive period of organogenesis.
Second Trimester: Most appropriate for various treatments like tooth extraction, filling, and canal treatment.
Third Trimester: Limited to emergency treatments; prolonged sitting may cause vena cava inferior syndrome.
Types of Treatments
Safe Treatments: Extractions, local anesthetic, root canal treatment, scaling, and root planning.
Emergency Cases: Treat tooth and gingival inflammation promptly to avoid adverse effects on the baby.
Recommendations for Oral Care During Pregnancy
Pregnancy-Safe Toothpaste
Selecting the right toothpaste during pregnancy is essential to maintain oral health while minimizing irritation or sensitivity. Pregnant patients should look for toothpastes that:
Are Free of Sodium Lauryl Sulfate (SLS): This ingredient can irritate sensitive oral tissues and potentially worsen canker sores.
Contain Fluoride: Fluoride helps prevent cavities, which is particularly important during pregnancy when hormonal changes can increase the risk of gum disease and tooth decay.
Are Gentle on Enamel: Toothpastes formulated for sensitive teeth can provide additional comfort for patients experiencing pregnancy-related sensitivity.
Advising patients to brush twice daily with a soft-bristled toothbrush and a pregnancy-safe toothpaste can help support oral health throughout pregnancy.
Pregnancy-Safe Mouthwash
A good mouthwash during pregnancy should be effective yet gentle, avoiding ingredients that may pose risks to the mother or baby. Key features to recommend include:
Alcohol-Free Formulas: Alcohol can be harsh on oral tissues and should be avoided.
Fluoride Options: Fluoride rinses can help strengthen enamel and prevent cavities.
Soothing Ingredients: Mouthwashes with natural ingredients like aloe vera or chamomile can help soothe irritated gums.
Patients experiencing morning sickness may also benefit from a mild mouthwash to neutralize acids and maintain a clean oral environment. Advise rinsing with water before using mouthwash to prevent further irritation.
The Role of Dentists in Safe Pregnancy
Dentists play a vital role in ensuring the safety of medications prescribed during pregnancy, particularly in dental care. It’s essential to evaluate every medication’s potential impact on both the mother and baby. To assist with this, DentalRx provides an invaluable resource for dental professionals to ensure safe prescribing practices during pregnancy.
To help in this endeavour, we have created the mobile and web application DentalRx. Dentists use DentalRx to research medications, including those used in pregnancy, so they may safely prescribe and ultimately provide better patient care.
Each prescribing monograph in the DentalRx app includes a dedicated section for Pregnancy and Lactation, offering dentists instant access to up-to-date safety information. The app also provides specific treatment guidelines for pregnant patients, enabling dental professionals to make informed decisions effortlessly, without relying on outdated or unclear resources.
By using DentalRx, dentists can confidently prescribe medications, safeguarding both maternal and fetal health while improving the overall quality of patient care. Ensure the safety of your pregnant patients by integrating DentalRx into your practice today!
Conclusion
Understanding the evidence for medication use in pregnancy and their application in dental practice is a crucial aspect of patient care. The well-being of both the mother and the unborn child depends on the dental professional’s knowledge and judgment. Always consult with healthcare providers and consider alternative therapies when appropriate.
Resources:
American Dental Association (ADA). (2023, June 22). Pregnancy and oral health. Retrieved from https://www.ada.org/resources/ada-library/oral-health-topics/pregnancy
Walling, A. D. (2006, September 15). Antibiotic use during pregnancy and lactation. American Family Physician, 74(6), 1035. Retrieved from https://www.aafp.org/pubs/afp/issues/2006/0915/p1035.html
U.S. Food and Drug Administration (FDA). (2024, October 1). FDA drug safety communication: FDA has reviewed possible risks of pain medicine use during pregnancy. Retrieved from https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-has-reviewed-possible-risks-pain-medicine-use-during-pregnancy
Yenen, Z., & Ataçağ, T. (2019). Oral care in pregnancy. Journal of Oral Health and Preventive Dentistry, PMC6883753. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6883753/
Lee, J. M., & Shin, T. J. (2017). Use of local anesthetics for dental treatment during pregnancy; safety for parturient. Korean Journal of Pain, PMC5564152. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5564152/
Kurien, S., Kattimani, V. S., Sriram, R. R., Sriram, S. K., Rao, V. K. P., Bhupathi, A., Bodduru, R. R., & Patil, N. N. (2013). Management of pregnant patient in dentistry. Journal of International Oral Health, PMC3768073. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3768073/
Ensuring Dental Safety for Pregnant Patients
Managing dental care for pregnant patients is a complex yet crucial responsibility. Dental professionals must navigate treatment options with caution, especially when prescribing medications. The goal of this article is to provide an evidence-based guide to facilitate safer and more effective treatment plans for pregnant patients.
Revised Drug Pregnancy Categories in Dental Practice
Previously, the FDA provided drug pregnancy categories for healthcare professionals to make decisions about drug therapy. These categories provided a framework for evaluating the risks and benefits of medication use during pregnancy.
In 2015, the Food and Drug Administration (FDA) eliminated the standard pregnancy category letters (A, B, C, D, and X) for prescription medications. The new recommendations now take the form of drug labeling that provides greater detail but also introduces increased complexity.
The FDA’s transition from pregnancy category letters to more comprehensive labeling requires dentists to assess medication risks carefully. This change reflects a need for a deeper understanding of medication safety in pregnancy.
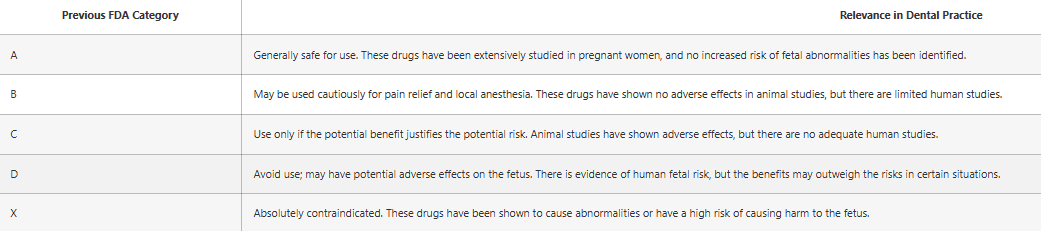
Following the FDA's changes, health professionals should no longer base their decisions on pregnancy categories. Instead, they should adopt a nuanced approach to each medication, carefully assessing all available evidence.
Continuing in this article, we will be summarizing the evidence that we have collected for your convenience.
Medications Commonly Used in Dental Practice
The following table from the 2012 Oral Health Care During Pregnancy Expert Workgroup is particularly helpful as a quick reference when prescribing medications for pregnant dental patients. It provides a concise overview of the commonly prescribed medications in dentistry.
Analgesics
Acetaminophen
May be used during pregnancy.
Oral pain can often be managed with non-opioid medication.
Acetaminophen with Codeine
During pregnancy, this medication should be used only when clearly needed.
It may slightly increase the risk of birth defects if used during the first two months of pregnancy.
Prescribed in high doses near the expected delivery date may harm the unborn baby.
To lessen the risk, prescribe the smallest effective dose for the shortest possible time.
Babies born to mothers who use this drug for a long time may develop severe (possibly fatal) withdrawal symptoms.
Aspirin
First trimester: Avoid use.
Second trimester (13–20 weeks): May use for a short duration (48–72 hours).
Second trimester (20–27 weeks): Limit use.
Third trimester: Avoid use.
Ibuprofen and Naproxen
Second trimester, after 20 weeks: Avoid use.
Third trimester: Avoid use.
Antibiotics
Amoxicillin, Cephalosporins, Clindamycin, Metronidazole, Penicillin
May be used during pregnancy.
Ciprofloxacin, Levofloxacin, Moxifloxacin
Avoid during pregnancy.
Tetracycline
Never use during pregnancy.
Anesthetics
Local Anesthetics with Epinephrine (e.g., Bupivacaine, Lidocaine, Mepivacaine)
May be used during pregnancy.
General Anesthesia
Consult a prenatal care health professional before use.
Limit duration of exposure to less than 3 hours, especially in the third trimester.
Antimicrobials
Cetylpyridinium Chloride Mouth Rinse, Chlorhexidine Mouth Rinse, Xylitol
May be used during pregnancy.
Use alcohol-free products during pregnancy.
Updates Since the Working Group
The list above was published in 2012 by the expert working group, and since then additional commentary has been provided on certain medications used in pregnancy.
Nitrous Oxide: It is recommended that pregnant individuals avoid exposure to nitrous oxide. The National Institute of Occupational Safety and Health (NIOSH), recommends exposure limits of N2O concentrations in dental operations to approximately 25 ppm during analgesia administration.
Meperidine: Meperidine should not be used in pregnant women before the onset of labor unless the physician determines that the potential benefits outweigh the associated risks. Safe use in pregnancy before labor has not been established relative to possible adverse effects on fetal development. Available data with DEMEROL Injection are insufficient to inform a drug-associated risk for major birth defects and miscarriage.
Morphine: Based on the studies reviewed, it is not known if morphine increases the chance of pregnancy-related problems such as preterm delivery (birth before week 37) or low birth weight (weighing less than 5 pounds, 8 ounces [2500 grams] at birth).
One case of high heart rate (tachycardia) in a near-term (36-week) fetus was described after a person who was pregnant was given morphine for kidney pain (renal colic). A person using morphine for chronic pain control in their third trimester of pregnancy was observed to have constriction in the blood vessels of the placenta, also known as placental vasoconstriction.
Bupivacaine, Mepivacaine: These local anesthetics should not be used in pregnant women before the onset of labor unless the physician determines that the potential benefits outweigh the possible risks. Fetal bradycardia with Mepivacaine & Bupivacaine is a potential risk.
Special Considerations in Dental Practice
Timing of Treatments
First Trimester: Avoid non-emergency treatments due to the sensitive period of organogenesis.
Second Trimester: Most appropriate for various treatments like tooth extraction, filling, and canal treatment.
Third Trimester: Limited to emergency treatments; prolonged sitting may cause vena cava inferior syndrome.
Types of Treatments
Safe Treatments: Extractions, local anesthetic, root canal treatment, scaling, and root planning.
Emergency Cases: Treat tooth and gingival inflammation promptly to avoid adverse effects on the baby.
Recommendations for Oral Care During Pregnancy
Pregnancy-Safe Toothpaste
Selecting the right toothpaste during pregnancy is essential to maintain oral health while minimizing irritation or sensitivity. Pregnant patients should look for toothpastes that:
Are Free of Sodium Lauryl Sulfate (SLS): This ingredient can irritate sensitive oral tissues and potentially worsen canker sores.
Contain Fluoride: Fluoride helps prevent cavities, which is particularly important during pregnancy when hormonal changes can increase the risk of gum disease and tooth decay.
Are Gentle on Enamel: Toothpastes formulated for sensitive teeth can provide additional comfort for patients experiencing pregnancy-related sensitivity.
Advising patients to brush twice daily with a soft-bristled toothbrush and a pregnancy-safe toothpaste can help support oral health throughout pregnancy.
Pregnancy-Safe Mouthwash
A good mouthwash during pregnancy should be effective yet gentle, avoiding ingredients that may pose risks to the mother or baby. Key features to recommend include:
Alcohol-Free Formulas: Alcohol can be harsh on oral tissues and should be avoided.
Fluoride Options: Fluoride rinses can help strengthen enamel and prevent cavities.
Soothing Ingredients: Mouthwashes with natural ingredients like aloe vera or chamomile can help soothe irritated gums.
Patients experiencing morning sickness may also benefit from a mild mouthwash to neutralize acids and maintain a clean oral environment. Advise rinsing with water before using mouthwash to prevent further irritation.
The Role of Dentists in Safe Pregnancy
Dentists play a vital role in ensuring the safety of medications prescribed during pregnancy, particularly in dental care. It’s essential to evaluate every medication’s potential impact on both the mother and baby. To assist with this, DentalRx provides an invaluable resource for dental professionals to ensure safe prescribing practices during pregnancy.
To help in this endeavour, we have created the mobile and web application DentalRx. Dentists use DentalRx to research medications, including those used in pregnancy, so they may safely prescribe and ultimately provide better patient care.
Each prescribing monograph in the DentalRx app includes a dedicated section for Pregnancy and Lactation, offering dentists instant access to up-to-date safety information. The app also provides specific treatment guidelines for pregnant patients, enabling dental professionals to make informed decisions effortlessly, without relying on outdated or unclear resources.
By using DentalRx, dentists can confidently prescribe medications, safeguarding both maternal and fetal health while improving the overall quality of patient care. Ensure the safety of your pregnant patients by integrating DentalRx into your practice today!
Conclusion
Understanding the evidence for medication use in pregnancy and their application in dental practice is a crucial aspect of patient care. The well-being of both the mother and the unborn child depends on the dental professional’s knowledge and judgment. Always consult with healthcare providers and consider alternative therapies when appropriate.
Resources:
American Dental Association (ADA). (2023, June 22). Pregnancy and oral health. Retrieved from https://www.ada.org/resources/ada-library/oral-health-topics/pregnancy
Walling, A. D. (2006, September 15). Antibiotic use during pregnancy and lactation. American Family Physician, 74(6), 1035. Retrieved from https://www.aafp.org/pubs/afp/issues/2006/0915/p1035.html
U.S. Food and Drug Administration (FDA). (2024, October 1). FDA drug safety communication: FDA has reviewed possible risks of pain medicine use during pregnancy. Retrieved from https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-has-reviewed-possible-risks-pain-medicine-use-during-pregnancy
Yenen, Z., & Ataçağ, T. (2019). Oral care in pregnancy. Journal of Oral Health and Preventive Dentistry, PMC6883753. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6883753/
Lee, J. M., & Shin, T. J. (2017). Use of local anesthetics for dental treatment during pregnancy; safety for parturient. Korean Journal of Pain, PMC5564152. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5564152/
Kurien, S., Kattimani, V. S., Sriram, R. R., Sriram, S. K., Rao, V. K. P., Bhupathi, A., Bodduru, R. R., & Patil, N. N. (2013). Management of pregnant patient in dentistry. Journal of International Oral Health, PMC3768073. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3768073/
Ensuring Dental Safety for Pregnant Patients
Managing dental care for pregnant patients is a complex yet crucial responsibility. Dental professionals must navigate treatment options with caution, especially when prescribing medications. The goal of this article is to provide an evidence-based guide to facilitate safer and more effective treatment plans for pregnant patients.
Revised Drug Pregnancy Categories in Dental Practice
Previously, the FDA provided drug pregnancy categories for healthcare professionals to make decisions about drug therapy. These categories provided a framework for evaluating the risks and benefits of medication use during pregnancy.
In 2015, the Food and Drug Administration (FDA) eliminated the standard pregnancy category letters (A, B, C, D, and X) for prescription medications. The new recommendations now take the form of drug labeling that provides greater detail but also introduces increased complexity.
The FDA’s transition from pregnancy category letters to more comprehensive labeling requires dentists to assess medication risks carefully. This change reflects a need for a deeper understanding of medication safety in pregnancy.
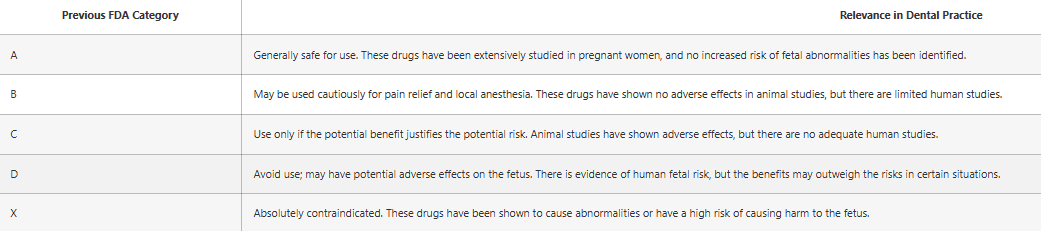
Following the FDA's changes, health professionals should no longer base their decisions on pregnancy categories. Instead, they should adopt a nuanced approach to each medication, carefully assessing all available evidence.
Continuing in this article, we will be summarizing the evidence that we have collected for your convenience.
Medications Commonly Used in Dental Practice
The following table from the 2012 Oral Health Care During Pregnancy Expert Workgroup is particularly helpful as a quick reference when prescribing medications for pregnant dental patients. It provides a concise overview of the commonly prescribed medications in dentistry.
Analgesics
Acetaminophen
May be used during pregnancy.
Oral pain can often be managed with non-opioid medication.
Acetaminophen with Codeine
During pregnancy, this medication should be used only when clearly needed.
It may slightly increase the risk of birth defects if used during the first two months of pregnancy.
Prescribed in high doses near the expected delivery date may harm the unborn baby.
To lessen the risk, prescribe the smallest effective dose for the shortest possible time.
Babies born to mothers who use this drug for a long time may develop severe (possibly fatal) withdrawal symptoms.
Aspirin
First trimester: Avoid use.
Second trimester (13–20 weeks): May use for a short duration (48–72 hours).
Second trimester (20–27 weeks): Limit use.
Third trimester: Avoid use.
Ibuprofen and Naproxen
Second trimester, after 20 weeks: Avoid use.
Third trimester: Avoid use.
Antibiotics
Amoxicillin, Cephalosporins, Clindamycin, Metronidazole, Penicillin
May be used during pregnancy.
Ciprofloxacin, Levofloxacin, Moxifloxacin
Avoid during pregnancy.
Tetracycline
Never use during pregnancy.
Anesthetics
Local Anesthetics with Epinephrine (e.g., Bupivacaine, Lidocaine, Mepivacaine)
May be used during pregnancy.
General Anesthesia
Consult a prenatal care health professional before use.
Limit duration of exposure to less than 3 hours, especially in the third trimester.
Antimicrobials
Cetylpyridinium Chloride Mouth Rinse, Chlorhexidine Mouth Rinse, Xylitol
May be used during pregnancy.
Use alcohol-free products during pregnancy.
Updates Since the Working Group
The list above was published in 2012 by the expert working group, and since then additional commentary has been provided on certain medications used in pregnancy.
Nitrous Oxide: It is recommended that pregnant individuals avoid exposure to nitrous oxide. The National Institute of Occupational Safety and Health (NIOSH), recommends exposure limits of N2O concentrations in dental operations to approximately 25 ppm during analgesia administration.
Meperidine: Meperidine should not be used in pregnant women before the onset of labor unless the physician determines that the potential benefits outweigh the associated risks. Safe use in pregnancy before labor has not been established relative to possible adverse effects on fetal development. Available data with DEMEROL Injection are insufficient to inform a drug-associated risk for major birth defects and miscarriage.
Morphine: Based on the studies reviewed, it is not known if morphine increases the chance of pregnancy-related problems such as preterm delivery (birth before week 37) or low birth weight (weighing less than 5 pounds, 8 ounces [2500 grams] at birth).
One case of high heart rate (tachycardia) in a near-term (36-week) fetus was described after a person who was pregnant was given morphine for kidney pain (renal colic). A person using morphine for chronic pain control in their third trimester of pregnancy was observed to have constriction in the blood vessels of the placenta, also known as placental vasoconstriction.
Bupivacaine, Mepivacaine: These local anesthetics should not be used in pregnant women before the onset of labor unless the physician determines that the potential benefits outweigh the possible risks. Fetal bradycardia with Mepivacaine & Bupivacaine is a potential risk.
Special Considerations in Dental Practice
Timing of Treatments
First Trimester: Avoid non-emergency treatments due to the sensitive period of organogenesis.
Second Trimester: Most appropriate for various treatments like tooth extraction, filling, and canal treatment.
Third Trimester: Limited to emergency treatments; prolonged sitting may cause vena cava inferior syndrome.
Types of Treatments
Safe Treatments: Extractions, local anesthetic, root canal treatment, scaling, and root planning.
Emergency Cases: Treat tooth and gingival inflammation promptly to avoid adverse effects on the baby.
Recommendations for Oral Care During Pregnancy
Pregnancy-Safe Toothpaste
Selecting the right toothpaste during pregnancy is essential to maintain oral health while minimizing irritation or sensitivity. Pregnant patients should look for toothpastes that:
Are Free of Sodium Lauryl Sulfate (SLS): This ingredient can irritate sensitive oral tissues and potentially worsen canker sores.
Contain Fluoride: Fluoride helps prevent cavities, which is particularly important during pregnancy when hormonal changes can increase the risk of gum disease and tooth decay.
Are Gentle on Enamel: Toothpastes formulated for sensitive teeth can provide additional comfort for patients experiencing pregnancy-related sensitivity.
Advising patients to brush twice daily with a soft-bristled toothbrush and a pregnancy-safe toothpaste can help support oral health throughout pregnancy.
Pregnancy-Safe Mouthwash
A good mouthwash during pregnancy should be effective yet gentle, avoiding ingredients that may pose risks to the mother or baby. Key features to recommend include:
Alcohol-Free Formulas: Alcohol can be harsh on oral tissues and should be avoided.
Fluoride Options: Fluoride rinses can help strengthen enamel and prevent cavities.
Soothing Ingredients: Mouthwashes with natural ingredients like aloe vera or chamomile can help soothe irritated gums.
Patients experiencing morning sickness may also benefit from a mild mouthwash to neutralize acids and maintain a clean oral environment. Advise rinsing with water before using mouthwash to prevent further irritation.
The Role of Dentists in Safe Pregnancy
Dentists play a vital role in ensuring the safety of medications prescribed during pregnancy, particularly in dental care. It’s essential to evaluate every medication’s potential impact on both the mother and baby. To assist with this, DentalRx provides an invaluable resource for dental professionals to ensure safe prescribing practices during pregnancy.
To help in this endeavour, we have created the mobile and web application DentalRx. Dentists use DentalRx to research medications, including those used in pregnancy, so they may safely prescribe and ultimately provide better patient care.
Each prescribing monograph in the DentalRx app includes a dedicated section for Pregnancy and Lactation, offering dentists instant access to up-to-date safety information. The app also provides specific treatment guidelines for pregnant patients, enabling dental professionals to make informed decisions effortlessly, without relying on outdated or unclear resources.
By using DentalRx, dentists can confidently prescribe medications, safeguarding both maternal and fetal health while improving the overall quality of patient care. Ensure the safety of your pregnant patients by integrating DentalRx into your practice today!
Conclusion
Understanding the evidence for medication use in pregnancy and their application in dental practice is a crucial aspect of patient care. The well-being of both the mother and the unborn child depends on the dental professional’s knowledge and judgment. Always consult with healthcare providers and consider alternative therapies when appropriate.
Resources:
American Dental Association (ADA). (2023, June 22). Pregnancy and oral health. Retrieved from https://www.ada.org/resources/ada-library/oral-health-topics/pregnancy
Walling, A. D. (2006, September 15). Antibiotic use during pregnancy and lactation. American Family Physician, 74(6), 1035. Retrieved from https://www.aafp.org/pubs/afp/issues/2006/0915/p1035.html
U.S. Food and Drug Administration (FDA). (2024, October 1). FDA drug safety communication: FDA has reviewed possible risks of pain medicine use during pregnancy. Retrieved from https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-has-reviewed-possible-risks-pain-medicine-use-during-pregnancy
Yenen, Z., & Ataçağ, T. (2019). Oral care in pregnancy. Journal of Oral Health and Preventive Dentistry, PMC6883753. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6883753/
Lee, J. M., & Shin, T. J. (2017). Use of local anesthetics for dental treatment during pregnancy; safety for parturient. Korean Journal of Pain, PMC5564152. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5564152/
Kurien, S., Kattimani, V. S., Sriram, R. R., Sriram, S. K., Rao, V. K. P., Bhupathi, A., Bodduru, R. R., & Patil, N. N. (2013). Management of pregnant patient in dentistry. Journal of International Oral Health, PMC3768073. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3768073/